INTRODUCTION
Pleomorphic adenoma is called as “mixed tumor” because it has both epithelial and connective tissue elements. It commonly affects parotid gland followed by minor salivary glands. About 450-750 minor salivary glands are present in the head and neck region. Highest concentration of these minor salivary glands has been described on the palate, particularly the junction of hard and soft palate. Most common minor salivary gland tumors occur at this site.1
In all 8-10% of salivary gland tumors arise in the palate. These tumors are malignant in 40-82% of cases.2-5 Tumors in minor salivary glands are more likely to be malignant than their counterparts in the major or paired glands.1-5 Salivary gland tumors can be divided into three types: benign, locally aggressive, malignant tumors with potentiated to metastatize.6 The most common locally aggressive tumor of the palate is the pleomorphic adenoma.6-8 Treatment of pleomorphic adenoma is aggressive local surgery with wide local excision extending at least V cm beyond the visible tumor margin. The aim of this case report is to present histopathologically diagnosed Pleomorphic adenoma of palate in a 24-year-old female, to emphasize its peculiar nature of growing slowly for over years to a size of 2x2 cm, and yet asymptomatic.
CASE REPORT
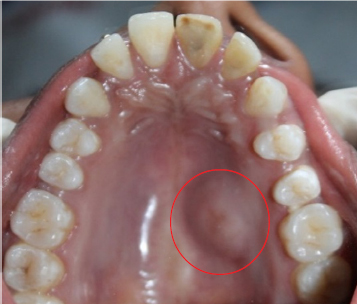
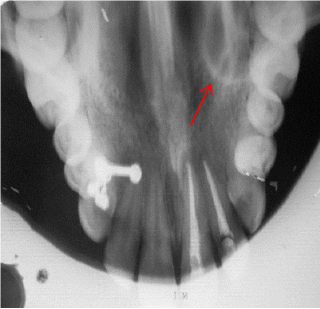
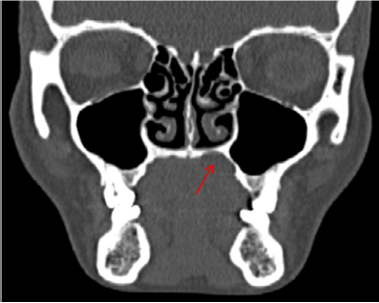
A 24 year old female pateint was referred to Department of Oral and Maxillofacial Surgery, Kamineni Institute of Dental sciences, narketpally with the chief complaint of a swelling at the left side of the palate since 7years (Figure 1). Her medical history was non-contributory and she denied drug allergy. She gave the history that the swelling had been there for 7years. Intraoral examination a well- defined solitary swelling is seen over left side of palate of size 2x2 cm approximately extending from left 1st premolar to left 2nd molar area anteroposteriorly and buccopalatally from midpalatine raphae to gingival margin. No discharge from swelling overlying palatal mucosa. The mucosa over the swelling appeared to be normal with well-defined borders with surrounding mucosa. On palpation it was non tender, firm in consistency, non-compressible, non-reducible did not show any fluctuation or pus discharge and fixed to underlying structure. There was no tooth displacement associated or mobility of tooth adjacent to the lesion. Intraoral peri-apical radiograph reveals no carious involvement of tooth, occlusal view reveals radiopaque lesion over left side (Figure 2). CT reveals bony erosion (Figure 3, 4 & 5). All blood counts were within normal limits. The probability of other clinical diagnosis of palatal abscess was completely ruled out. There was no lymphadenopathy.
|
Figure 1: Palatal swelling is seen over left side of the hard palate.
Click here to view |
|
Figure 2: Occlusal radiograph showing radiopaque lesion over the left side of the hard palate.
Click here to view |

|
Figure 3: CT-axial view showing bony erosion seen over the left side of palate.
Click here to view |
|
Figure 4: CT- coronal view showing bony erosion seen over the left side of palate.
Click here to view |

|
Figure 5: CT- sagittal view showing bony erosion seen over the left side of palate.
Click here to view |
MANAGEMENT
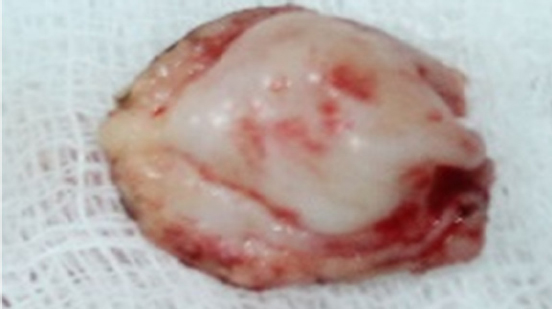
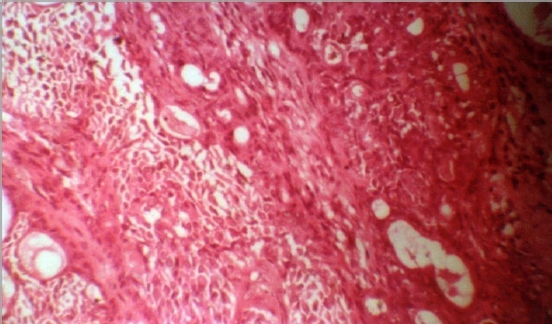
Under general anesthesia with nasotracheal intubation, Local anesthetic solution containing 1:80000 adrenaline was infiltrated around the lesion. Dingmans retractor was placed to increase the access to lesion in the palate. Mucosa around the lesion was marked (Figure 6) & incised using the surgical blade approximately 1cm away. Palatal mucosa is reflected with periosteal elevator and wide excision of the lesion was done. Haemostasis was achieved with electro cautery. The lesion was excised along with its fibrous capsule (Figure 7). During surgery, the tumor was found to be embedded in a bony cavity in the palate, possibly due to erosion from the growing lesion. After the tumor was removed, curettage of the walls and floor of the bony cavity was done using a bur under copious sterile normal saline irrigation, to ensure that no remnants of the lesion remained to cause recurrence. There was no communication between the bony cavity in the hard palate and the nasal cavity. Chlorhexidine gauze dressing given and it is stabilised with palatal acrylic plate (Figure 8). Histologically, H & E stained section showed mixture of polygonal epithelial and spindle-shaped myoepithelial elements in a variable background stroma. Epithelial elements are arranged in duct-like structures, sheets, clumps or interlacing strands and consist of polygonal, spindle or stellate-shaped cells (Figure 9). Two months follow up showed satisfactory healing (Figure 10).

|
Figure 6: Mucosa around the lesion marked
Click here to view |
|
Figure 7: Excised mass from the lesion
Click here to view |

|
Figure 8: Stabilisation of the defect with palatal plate.
Click here to view |
|
Figure 9: Histopathological report of the biopsy specimen shows mixture of polygonal epithelial and spindle shaped myoepithelial elements.
Click here to view |

|
Figure 10: Two months post operative healing.
Click here to view |
DISCUSSION
Tumors occurring in the small salivary glands account for 20-40% of all salivary gland tumors, precisely 22%, according to Spiro.8 The smaller the salivary gland that is affected, the more likely it is to trigger a malignant tumor.9 Mixed tumor of the minor salivary glands affects mostly patients in their fourth to sixth decades, with a predominance of females. Clinically pleomorphic adenoma presents as a slow-growing, asymptomatic, unilateral firm mass that may become large if is untreated. When originating in the minor salivary glands, in most cases it occurs on the soft and hard palate due to the highest concentration of salivary glands there and is typically a firm or rubbery submucosal mass without ulceration or surrounding ulceration.10
Histologically, it is highly variable in appearance. Classically it is biphasic and is characterized by a mixture of polygonal epithelial and spindle-shaped myoepithelial elements in a variable background stroma that may be mucoid, myxoid, cartilaginous or hyaline.11 Epithelial elements may be arranged in duct-like structures, sheets, clumps or interlacing strands and consist of polygonal, spindle or stellate-shaped cells. Areas of squamous metaplasia and epithelial pearls may occur. The tumor is not enveloped, but is surrounded by a fibrous pseudocapsule of varying thickness. The tumor extends through normal glandular parenchyma in the form of finger-like pseudopodia, but this is not a sign of malignant transformation.11, 12 Each tumor shares with others the essential feature of being composed of both epithelial and mesenchymal-like tissues. The proportion of each of these elements varies widely and one or the other is often predominant. The “cellular” type of pleomorphic adenoma is one in which the epithelial element predominates, whereas the “myxoid” type is composed mostly of a myxomatous or myxochondromatous mesenchymal-like element. The “mixed” type is a classic form. Distinctive epithelial cell types include spindle, clear, squamous, basaloid, cuboidal, plasmacytoid, oncocytic, mucous and sebaceous.11, 13, 14
The diagnosis of pleomorphic adenoma is established on the basis of history, physical examination, cytology and histopathology. An incisional biopsy must be performed to determine the proper management regimen and treatment.15, 16 Computed tomography scan and MRI can provide information on the location and size of the tumor and extension to surrounding superficial and deep structures.17 Fine-needle aspiration cytology and incisional biopsy can aid in the diagnosis. The treatment is strictly wide local excision with the
removal of periosteum or bone if they are involved.2,18
The differential diagnosis for this case includes palatal abscesses, odontogenic and non-odontogenic cysts, soft tissue tumors such as fibroma, lipoma, neurofibroma, neurilemmoma, and lymphoma as well as other salivary gland tumors. Palatal abscess could be ruled out by clinical examination since the source of a palatal abscess, which is typically a nonvital tooth in the vicinity or a localized periodontal defect, was not found. Both odontogenic and non-odontogenic cysts could be ruled out at the time of exploration into the mass since it did not demonstrate a cystic nature. Palatal tissues contain components of soft tissue and harbor minor salivary gland tissues. Myoepithelioma is a benign epithelial salivary gland tumor, having plasmacytoid or spindled myoepithelial cells.18 Differentiation between benign and malignant tumors is not possible without histopathology. Enucleation of pleomorphic adenomas leads to a high recurrence rate, so it should be avoided. Surgical exposure of the tumor or tumor capsule risks spillage and dramatically increases the risk of recurrence, but pleomorphic adenomas of the minor glands have little propensity for recurrence (a recurrence rate of 2 to 44%, but mainly of the parotid gland). Recurrent pleomorphic adenomas often form multiple, separate nodules within the remaining salivary gland, periparotid tissues, dermis, or scar tissue even a few or dozen years after the initial surgery. Inadequate surgical procedure was reported to be the main cause of failure. The most frequent surgical issues are pseudopodia, capsular penetration and tumor rupture. Distant metastases are also possible.2, 19
Fifty percent of all tumors derived from the minor salivary glands are reported to be malignant, adenoid cystic carcinoma being the most malignant tumor. Pleomorphic adenomas of the minor salivary glands, like those on the palate, buccal mucosa or lip, sometimes lack encapsulations and may mix into normal host tissue as tumor growth; hence a wide excision is necessary even if previous biopsies report benign nature. If pleomorphic adenoma is located in the superficial lobe of the parotid gland, an effective way of treatment is superficial parotidectomy. When the tumor is located in the deep lobe of the parotid gland, the method of choice is total parotidectomy.20, 21
Reconstruction of the palate is a challenging endeavor. As with any defect, thinking about the goals of reconstruction from both a functional and esthetic point of view will help decide which approach is most suitable for the patient. Soft tissue defects of the hard palate are essentially a nonissue, as the hard palate can be left to granulate. Bony defects in a dentate patient can be treated conservatively with an obturator. Bony defects of the upper alveolar ridge will cause a significant cosmetic and functional deformity, and therefore free tissue transfer techniques will augment the anterior projection of the face and the soft tissue can be used to seal the oral cavity from the nose. Each technique has its advantages and disadvantages. The goal of maintaining speech, swallowing and anterior facial projection should be kept at the forefront of each surgeon’s mind when approaching these difficult cases.22
CONCLUSION
This case represents a classic example of pleomorphic adenoma of the palate. Successful treatment begins with an appropriate referral and a biopsy-proven diagnosis. Computed tomography aids in evaluating the extent of the lesion and in guiding the surgical strategy. A long-term follow- up is warranted because of the risk of recurrence even several years after the initial excision. Most salivary gland tumors should be dissected due to the possibility of becoming malignant. Wide excision with negative margins is the optimal strategy for the management of pleomorphic adenomas due to occasional lack of encapsulation, mixing into normal host tissue and pseudopodia. A histopathological biopsy should be routinely taken after the excision of the neoplastic lesion. Adequate surgical excision corresponds with lower risk of recurrence.
