INTRODUCTION
Bipolar mood disorder is a form of depressive disorder that used to be called manic depressive illness. Most patients display an extreme cycling of moods once every few years. However, some people, described as “rapid cyclers,” experience mood swings at least 4 times per year, a situation more resistant to conventional treatment.1 This psychiatric illness affects approximately 1% to 2% of the general population, with no difference in prevalence among men and women.2, 3
This disorder has 2 major types-bipolar disorder I and bipolar disorder II. Bipolar disorder I is defined by episodes of depression and the presence of mania, whereas bipolar disorder II is characterized by episodes of depression and hypomania.
During depressive episodes, many patients exhibit a distinct decline in the level of oral hygiene, along with a rise in dental caries and periodontal disease, which often progress to an unmanageable situation.4-6 Conversely, during manic periods, overzealous use of oral health aids such as toothbrushes and floss may be associated with a corresponding increase in the incidence and severity of cervical abrasion, as well as occasional mucosal or gingival lacerations.7, 8 Unfortunately, medical pharmacotherapy for bipolar disorder can result in moderate to severe xerostomia, which further compounds the severity of any dental disease.9-11
In recent years, several new medications have been developed for even more effective management of bipolar disorder, including anticonvulsants such as valproic acid.12 This particular medication is being used more frequently as a first-choice treatment for mania because it is safer than lithium. Some of the common adverse effects of valproic acid include tiredness, tremor, sedation, and gastrointestinal disturbances. In addition, about 10% of the users experience reversible hair loss and rarely gingival enlargement.13
Drug-induced gingival enlargement is the term now used to describe medication-related gingival hypertrophy or hyperplasia, a condition commonly induced by three main classes of drugs: anticonvulsants, antihypertensive calcium channel blockers, and immune suppressants. Among the anticonvulsants, gingival enlargement is seen mostly with phenytoin (diphenylhydantoin). The other anticonvulsants that have the gingival enlargement effect are vigabatrin, sodium valproate, primidone, and phenobarbital.14
CASE REPORT
A 42 year old male patient presented to the dental outpatient department of periodontology, Govt. dental college and Hospital, Aurangabad with a complaint of mobile teeth in lower front region of jaw since 6-8 months and foul odour from mouth. Case history revealed that patient is on active psychiatric medication for bipolar mood disorder i.e., Tab. sodium valproate 500mg OD, Tab. Respiridone 1mg HS OD, since last 12 years.
At age of 5 years, he was diagnosed with hydrocephalus, which was arrested on its own without treatment, he had 5 attack of depression in year from 1995-2001 and he suffered from hypomania in 2001-2002. History also includes, impairment in social/occupational areas of functioning, diminished vision of left eye and abnormal gait.
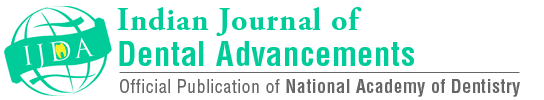
Clinical examination showed gingival enlargement involving interdental papilla with 15, 13, 12, 11, 21, 22, 23, 32 extending to facial, lingual gingival margins and attached gingiva with 14, 24, 25, 35, 34, 33, 43, 44, 45. Gingiva was pink in colour, erythematous with rolled out margins and loss of gingival scalloping (Figure 1). Cervical abrasion and sensitivity to hot and cold in 22, 23, 33, 34, 43, 44, dental caries with 15, 16 root pieces with 26, 27; and extrusion with 37, 48. Grade I mobility with 24, 25, 32, 42, 48 and Grade II mobility with 41 with generalised pockets and recession was also observed. Oral malodor was present. Oral hygiene was poor. Plaque index and Gingival Index were recorded. The radiologic examination showed generalized bone loss. Based on clinical and radiological examination patient was diagnosed as generalised chronic moderate periodontitis.

|
Figure 1: Pre-operative picture showing poor oral hygiene.
Click here to view |
Firstly, Full mouth disinfection (FMD) was carried out. In which chair side mouth rinsing was done by the patient with a 0.2% chlorhexidine solution for 2 minutes. After that, fullmouth scaling and root planing of entire dentition was done within 24 hours. This was followed by an additional subgingival irrigation of all pockets with a 1% chlorhexidine gel. Furthermore, patient was advised for tongue cleaning with 1% chlorhexidine gel. The standard oral hygiene instructions were given which included interdental plaque control by dental floss and use of interdental brushes, antiseptic mouthwash (0.2% chlorhexidine), tooth brushing and cleaning of the dorsum surface of tongue twice a day. As the patient was in stable condition since last 12 years when he was shifted on sodium valproate, the drug was not replaced as advised by the physician. Root pieces 26, 27 were extracted after taking physician consent and restoration 15, 16 was done after excavating the dental caries. The anterior mandibular mobile teeth were splinted. Desensitising agent was prescribed.
After 6 weeks follow-up, there was reduction in Plaque index, Gingival Index, probing pocket depth (Figure 2). Based on the clinical finding, local drug delivery was performed using tetracycline- impregnated fibrillar collagen that contains 25 mg pure fibrillar collagen containing approximately 2 mg of evenly impregnated tetracycline Hydrochloride (HCl) (Figure 3). There was reduction in gingival enlargement after 3 months follow-up (Figure 4).

|
Figure 2: Post-operative picture after 6 weeks
Click here to view |
|
Figure 3: Local drug delivery using tetracycline fibers
Click here to view |

|
Figure 4: Post-operative picture after 3 months.
Click here to view |
DISCUSSION
There is no cure for bipolar disorder, but a 3- pronged treatment approach can be taken to the management of this illness: pharmacotherapy, psychotherapy and life adjustment skills education. Valproic acid is an anticonvulsant used in the treatment of epilepsy and bipolar disorder, as well as other psychiatric conditions requiring the administration of a mood stabilizer. It can be used to control acute episodes of mania. Other medications include antipsychotics such as risperidone and olanzapine, both of which display fewer side effects and less interference with cognitive functioning than lithium. Antidepressant medications such as tricyclic antidepressants and selective serotonin reuptake inhibitors may be added to the therapeutic regimen in some instances to assist in the management of the depressive phase. Electroconvulsive therapy (ECT) may be indicated for patients with severe depressive episodes that are refractory to medication. With ECT, a central nervous system seizure is created by means of an electric current; the seizure is thought to accentuate the responsiveness of neuronal membranes to norepinephrine and serotonin. It is important for the anaesthetist or dental consultant to assess the patient’s dentition before ECT to rule out any loose or broken teeth that could be aspirated during the treatments.15 As well, partial or complete dentures must also be identified. A bite block is generally placed between the teeth by the anaesthetist to protect both the teeth and the tongue from the clenching that occurs upon stimulation of the masseter muscles. Dental hygiene is neglected, and any existing prostheses may become ill fitting and may be discarded. With reduced salivary flow there is a rapid increase in the degree of dental deterioration, mucosal dryness and dysphagia. Patients often experience a sharp increase in rampant cervical caries not only because of the anticholinergic effects of lithium and other psychotropic medications, but also because they use candies or sweetened beverages to provide some form of oral lubrication.16
The treatment options for drug-induced gingival enlargement are based on the medication being used and the clinical presentation of the individual case. Dentists first consider the nonsurgical approach including the removal of local factors and replacement of the offending drug after consulting the physician. If the nonsurgical approach is not effective, periodontal surgery i.e Gingivectomy or periodontal flap is performed. Afterwards patient is kept on oral hygiene maintainence programme which include tooth brushing, interdental plaque control by interdental brushes and dental floss, antiseptic mouth rinse and tongue cleaning twice a day. The onestage, fullmouth disinfection concept results in significant additional clinical improvements with nonsurgical periodontal therapy.17 Therefore, it is beneficial both for the clinician and the patient as it provides a better outcome of the mechanical debridement, reduced need for surgery, and more efficient time management, with less absence from work for the patient. In this case, after the consultation with the physician, the drug was not replaced as the patient was in stable condition since last 12 years when he was shifted on sodium valproate.
Tetracyclines have been used extensively in the treatment of periodontal disease since many years. Tetracyclines are semi-synthetic chemotherapeutic agents which are bacteriostatic in action and hence are effective against rapidly multiplying bacteria. Tetracycline and its derivatives have been used systemically as well as locally in the treatment of periodontal disease. Local drug delivery avoids most of the problems associated with systemic therapy by limiting the drug to its target site with little or no systemic uptake. Tetracyclines have been incorporated into a variety of delivery systems (nonresorbable or bioresorbable) for insertion into periodontal pockets. These include hollow fibers (Goodson et al., 1979), ethylene vinyl acetate copolymer fibers (Goodson et al., 1983), ethyl cellulose fibers (Friedman and Golomb, 1982), acrylic strips (Addy et al., 1982), collagen preparations (Minabe et al., 1 989), and hydroxypropyl cellulose films (Noguchi et al., 1984).18
Through encouragement, motivation and education about improving health, the dental practitioner can enhance the sense of identity and self-esteem for patients with bipolar disorder, there by contributing in some degree to their psychological rehabilitation.19 The overall goal of treatment planning must incorporate the maintenance of oral health, comfort and function as well as the prevention and control of specific oral disease. Before commencing any treatment, the dental practitioner should consult with the patient’s physician or psychiatrist to confirm or update information about the current medication regimen, degree of compliance, ability to provide consent and overall psychological profile. The dental practitioner should also be aware that depressed patients may be uncooperative for even simple routine procedures.
CONCLUSION
The lifetime management of patients with bipolar disorder is challenging, because of the dynamic, chronic, and fluctuating nature of this disease. Pharmacologic treatment is the mainstay of treatment for patients with bipolar mood disorder. Most oral health professionals have limited experience in providing care for people with bipolar mood disorder because of its 1-2% of prevalence rate. Oral health care requirements in the present case include treatment of dental caries, cervical abrasions, drug- induced gingival enlargement, chronic periodontitis and halitosis. Carious teeth were restored, desensitising agents were prescribed for sensitivity where cervical abrasion were present as they were not restorable. In present case xerostomia was absent but for halitosis proper tongue cleaning and mouthwash was advised. For drug induced gingival enlargement and periodontitis full mouth disinfection followed by local drug delivery using tetracycline fibre was done which resulted in the reduction of plaque, gingivitis, probing pocket depth and gingival enlargement and then patient was kept on oral hygiene maintenance programme.